Osteoarthritis
This serious, painful condition is the most common form of arthritis and can affect any joint.

Osteoarthritis is a degenerative joint disease that can affect the many tissues of the joint. It is by far the most common form of arthritis, affecting more than 32.5 million adults in the United States, according to the Centers for Disease Control and Prevention.
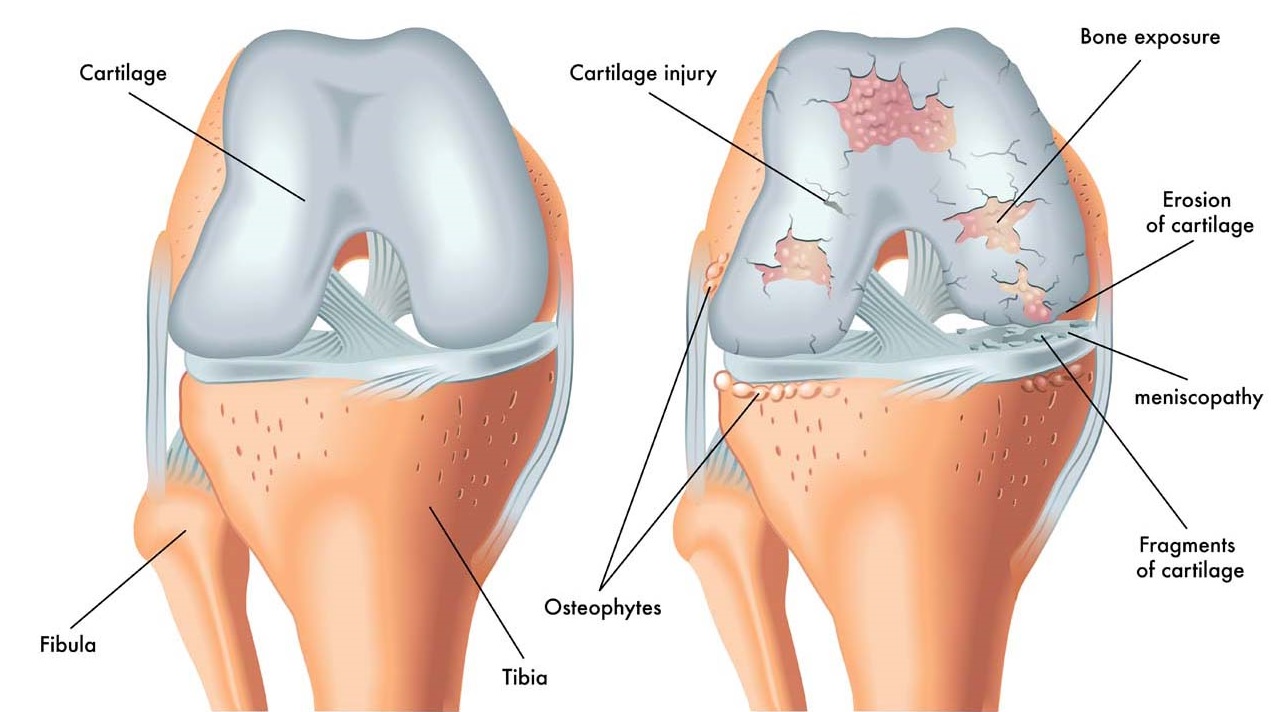
Historically, osteoarthritis (OA) was known as a “wear and tear” condition, generally associated with aging. But we know now that it is a disease of the entire joint, including bone, cartilage, ligaments, fat and the tissues lining the joint (the synovium). Osteoarthritis can degrade cartilage, change bone shape and cause inflammation, resulting in pain, stiffness and loss of mobility.
OA can affect any joint, but typically affects hands, knees, hips, lower back and neck. Its signs and symptoms typically show up more often in individuals over age 50, but OA can affect much younger people, too, especially those who have had a prior joint injury, such as a torn ACL or meniscus. It typically develops slowly over time, but after such an injury, it can develop much more rapidly, within just a few years. OA is not an inevitable aging disease; some people never develop it.
There is no cure for OA, but there are ways to manage OA to minimize pain, continue physical activities, maintain a good quality of life and remain mobile.
Causes
Factors that may contribute to the development of OA include
- Age. The risk of developing OA increases with age and symptoms generally, but not always, appear in people over 50.
- Joint injury. A bone fracture or cartilage or ligament tear can lead to OA, sometimes more quickly than in cases where there is not an obvious injury.
- Overuse. Using the same joints over and over in a job or sport can result in OA.
- . Excess weight adds stress and pressure on a joint, plus fats cells promote inflammation.
- Musculoskeletal abnormalities. Malalignment of bone or joint structures can contribute to faster development of OA.
- Weak muscles. If muscles don’t provide adequate joint support, poor alignment can result, which can lead to OA.
- Genetics. People with family members who have OA are more likely to develop it.
- Gender. Women are more likely to develop OA than men.
- Environmental Factors. Modifiable environmental risk factors include things like someone’s occupation, level of physical activity, quadriceps strength, presence or absence of prior joint injury, obesity, diet, sex hormones, and bone density.
Symptoms
Symptoms tend to build over time rather than show up suddenly. They include
- Pain or aching in a joint during activity, after long activity or at the end of the day.
- Joint stiffness usually occurs first thing in the morning or after resting.
- Limited range of motion that may go away after movement.
- Clicking or popping sound when a joint bends.
- Swelling around a joint.
- Muscle weakness around the joint.
- Joint instability or buckling (as when a knee gives out).
OA may affect different parts of the body in different ways.
- Hips. Pain in the groin area or buttocks and sometimes on the inside of the knee or thigh.
- Knees. A “grating” or “scraping” feeling when moving the knee.
- Fingers. Bony growths (spurs) at the edge of joints can cause fingers to become swollen, tender and red, sometimes with pain at the base of the thumb.
- Feet. Pain and tenderness in the big toe, with possible swelling in the ankles or toes.
Potential Consequences
Pain, reduced mobility, side effects from medications and other factors associated with osteoarthritis can lead to health complications that are not caused by the disease itself.
Obesity, Diabetes and Heart Disease
Painful joints, especially in the feet, ankles, knees, hip or back, make it harder to exercise. But physical activity is not only key to managing OA symptoms, it also can help prevent weight gain, which can lead to obesity. Being overweight or obese can lead to the development of high cholesterol, type 2 diabetes, heart disease and high blood pressure.
Falls
Research indicates people with OA experience more falls and risk of fracture than those without OA. Although study results vary, some research shows they may have up to 30% more falls and have a 20% greater risk of fracture. Having OA can decrease function, weaken muscles, affect overall balance, and make falls more likely, especially among those with OA in knees or hips. Side effects from pain medications, such as dizziness, can also contribute to falls.
Diagnosis
Medical history, a physical examination and lab tests help to make up the OA diagnosis.
A primary care doctor may be the first person you talk to about joint pain. The doctor will review your medical history, symptoms, how the pain affects activities, as well as your medical problems and medication use. He or she will also look at and move your joints and may order imaging. These tests help to make the diagnosis:
- Joint aspiration – After numbing the area, a needle is inserted into the joint to pull out fluid. This test will look for infection or crystals in the fluid to help rule out other medical conditions or other forms of arthritis.
- X-rays can show joint or bone damage or changes related to osteoarthritis.
- Magnetic resonance imaging (MRI) gives a better view of cartilage and other parts of the joint.
There is no cure for OA, but medication, assistive devices and other therapies that don’t involve drugs can help to ease pain
Massage Can Help

Pain Relief: Massage can help reduce pain associated with osteoarthritis by releasing tension in muscles and promoting relaxation. This can lead to decreased muscle spasms and improved joint mobility.
Improved Range of Motion: Osteoarthritis can restrict movement in affected joints. Massage therapy can help improve flexibility and range of motion by loosening tight muscles and increasing blood flow to the affected areas.
Reduced Inflammation: While massage doesn’t directly treat the underlying inflammation in osteoarthritis, it can help improve circulation, which may reduce inflammation in the joints and surrounding tissues.
Stress Reduction: Living with osteoarthritis can be stressful due to pain and limitations in movement. Massage therapy promotes relaxation and reduces stress, which can help manage the psychological impact of the condition.
Enhanced Well-being: Overall, receiving massage therapy can improve the quality of life for individuals with osteoarthritis by providing relief from pain and discomfort, promoting better sleep, and increasing feelings of well-being.
However, it’s important to note that massage therapy should be used as part of a comprehensive treatment plan for osteoarthritis, including other interventions such as exercise, medication, and lifestyle modifications. Additionally, individuals with osteoarthritis should consult with their healthcare provider before starting any new treatment, including massage therapy, to ensure it is safe and appropriate for their specific condition.